Almost everyone has felt that sudden, sharp pain of a mouth sore. These small but mighty lesions, known as oral ulcers or canker sores, can make talking and eating a miserable experience. While most are harmless and heal on their own, you might wonder why you keep getting them.
The truth is, oral ulcers have many different triggers. Therefore, understanding the root cause is the first step to finding lasting relief. This guide breaks down the common reasons for these painful sores and shows you how to stop them.
What Are Oral Ulcers?
Oral ulcers are open sores that occur on the mucous membrane inside the mouth. They are typically round or oval with a white, yellow, or gray center and a red border. Most ulcers heal on their own within 7 to 14 days, though some may persist longer.
What’s Causing Your Oral Ulcers?
The reasons for mouth sores can range from simple daily habits to more complex health issues. Here are the most common culprits.
1. Everyday Triggers and Minor Injuries
First, let’s look at the most frequent causes. Many oral ulcers are simply the result of:
- Accidental Bites: Biting your cheek or tongue is a classic trigger.
- Dental Appliances: The sharp edges of braces or dentures can rub against your mouth.
- Aggressive Brushing: Brushing too hard can easily damage the delicate lining of your mouth.
- Food Sensitivities: In addition, spicy, salty, or acidic foods can irritate your mouth and lead to sores.

2. Stress and Hormonal Changes
Your body often responds to stress in physical ways. For instance, periods of high stress or hormonal shifts (like those during a woman’s menstrual cycle) are well-known triggers for canker sore outbreaks.

Traumatic ulcer due to teeth
3. Nutritional Deficiencies
Sometimes, what’s missing from your diet can show up in your mouth. A lack of key nutrients is a common cause of recurrent oral ulcers. Specifically, deficiencies in:
- Vitamin B12
- Iron
- Folic Acid

Tongue ulcer due to vit B deff. with angular cheilitis
4. Underlying Health Conditions
In some cases, persistent oral ulcers can be a sign that something else is going on in your body. They are a known symptom of conditions like:
- Celiac disease and Crohn’s disease.
- Autoimmune disorders (like Behçet’s disease or Lichen Planus) where the body attacks its own tissues.
- Viral infections, such as the herpes simplex virus (cold sores).
5. Food Sensitivities
- Spicy, acidic, or salty foods can irritate the mouth lining.
6. Underlying Health Conditions
- Conditions like celiac disease, Crohn’s disease, or Behçet’s disease
- Autoimmune disorders

Behcet’s disease
7. Infections
- Viral infections like herpes simplex virus (cold sores), EBV and Coxsackie virus.

Stomatitis due to HSV
- Bacterial or fungal infections like candidiasis.
Oral candidiasis
- Syphilitic ulcers are typically painless with lymphadenopathy present.
8. Cancers
- Chronic, painless ulcers with red/white patches are suggestive of squamous cell carcinoma or premalignant dysplasias.
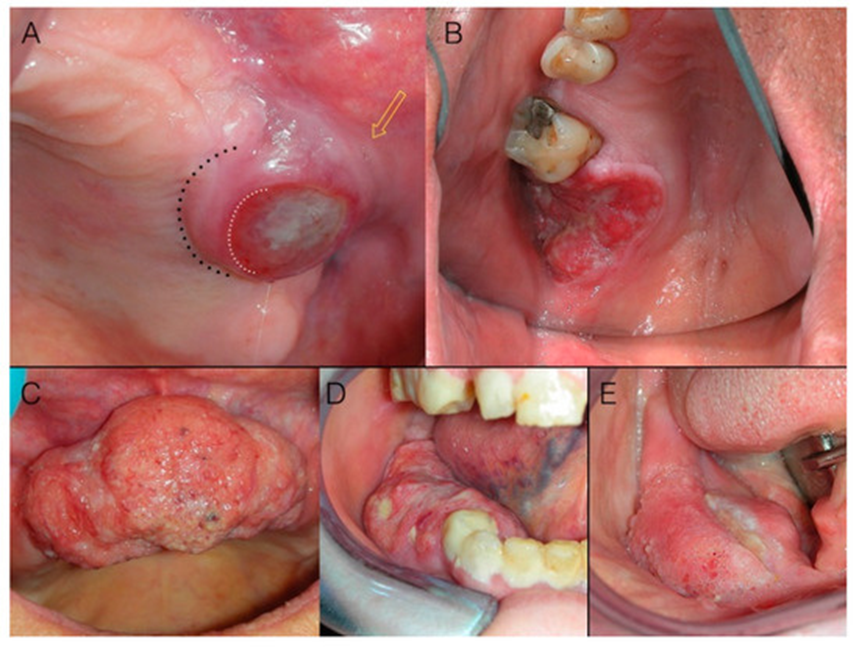
Squamous cell carcinoma of the gingiva appearing as an exophytic mass
9. Dermatologic diseases
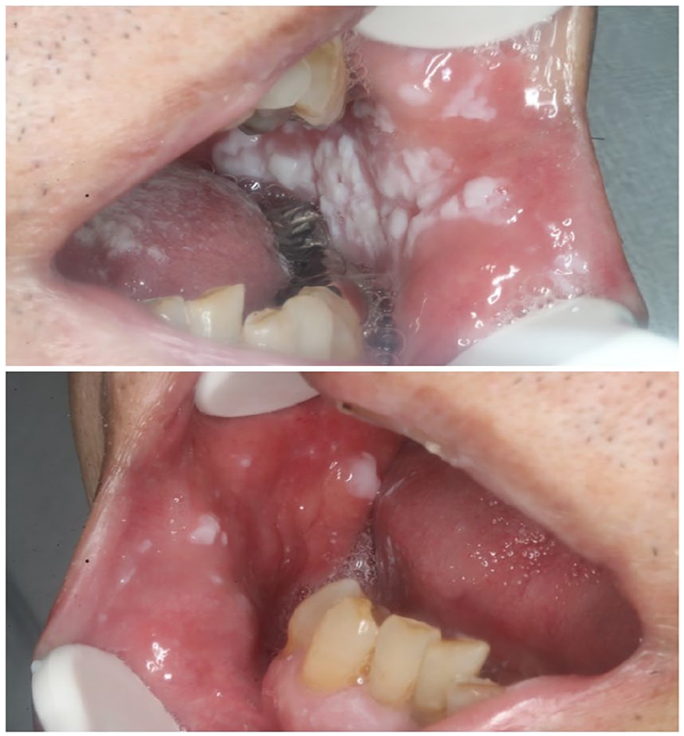
Lichen Planus
- Chronic inflammatory condition
- Reticular (lace-like) or erosive (ulcerative) lesions in the mouth
- T-cell-mediated autoimmune condition
Pemphigus Vulgaris
- Autoimmune blistering disease
- Oral ulcers often precede skin involvement
- Positive Nikolsky’s sign
Mucous Membrane Pemphigoid
- Chronic autoimmune blistering disorder involving oral mucosa
- Desquamative gingivitis common
How to Treat Painful Oral Ulcers
While most minor ulcers heal in a week or two, you don’t have to just suffer through the pain.
Simple Home Remedies for Fast Relief:
- Salt Water Rinse: Mix half a teaspoon of salt in a glass of warm water and swish it around your mouth. This helps clean the area and reduce pain.
- Avoid Trigger Foods: Stay away from anything spicy, acidic, or crunchy that could irritate the sore.
- Use a Soft Toothbrush: Be gentle when you brush to avoid further injury.
Over-the-Counter Solutions:
For more significant discomfort, you can find helpful products at your local pharmacy. For example, look for:
- Numbing Gels or Pastes: These products (often containing benzocaine) create a temporary protective barrier over the sore.
- Antiseptic Mouthwashes: A rinse can help keep the ulcer clean and prevent a secondary infection.
For more expert advice, you can visit a trusted source like the Mayo Clinic’s page on canker sores.
When You Absolutely Must See a Doctor
A typical canker sore is not a cause for panic. However, you should see a doctor or dentist if:
- An ulcer lasts for more than three weeks.
- The sores are unusually large or extremely painful.
- You get new ulcers before the old ones have healed.
- The ulcers are accompanied by a high fever or swollen glands.
These can be signs of a more serious issue that needs a proper diagnosis. If stress is a major trigger for you, check out our guide to simple stress-reduction techniques.
In conclusion, while oral ulcers are a common nuisance, you don’t have to let them control your life. By identifying your triggers, practicing good oral hygiene, and seeking medical advice for persistent sores, you can significantly reduce their frequency and impact.

