
Ear pain, medically known as otalgia, is a frequent and often distressing condition that can disrupt daily life. While it can affect anyone, it’s particularly common in children. The discomfort might be a fleeting annoyance or a sign of an underlying health issue. This updated guide explores the various causes of ear pain, associated symptoms, and the most effective and current treatment strategies.
What’s Causing That Ear Pain?
Pain in the ear can stem from issues within the ear itself (primary otalgia) or be referred from another part of the body (secondary otalgia).
According to the Mayo Clinic, ear infections are especially common in children.
Direct Causes Originating in the Ear
- Ear Infections (Otitis): Infections are a primary culprit behind ear pain.
- Otitis Media (Middle Ear Infection): Often following a cold or respiratory infection, fluid buildup behind the eardrum can lead to infection. This is the most common cause of ear pain in children.
- Otitis Externa (Swimmer’s Ear): This infection of the outer ear canal can be caused by water trapped in the ear, creating a breeding ground for bacteria. Using cotton swabs or having skin conditions like eczema in the ear can also increase the risk.
- Earwax Buildup: An accumulation of earwax can block the ear canal, causing discomfort, a feeling of fullness, and even temporary hearing loss.
- Barotrauma: Changes in air pressure during activities like flying, diving, or driving in the mountains can create a painful imbalance between the pressure in your middle ear and the outside environment.
- Foreign Objects: Especially in young children, items like beads, small toys, or food can get lodged in the ear canal, leading to pain and potential injury.
Indirect Causes: When the Pain is Referred
The ear shares nerves with many other parts of the head and neck, meaning pain can originate elsewhere and still be felt in the ear. Common sources of this “referred pain” include:
- Dental Problems: Cavities, infected teeth, or gum infections can radiate pain to the ear.
- Temporomandibular Joint (TMJ) Disorders: Issues with the jaw joint, often worsened by chewing, can be a significant source of referred ear pain.
- Sinus Infections (Sinusitis): Pressure from a sinus infection can cause a dull ache in the ears.
- Sore Throat and Tonsillitis: Infections in the throat can lead to ear pain due to shared nerve pathways.
- Nerve Irritation: Conditions like trigeminal neuralgia (chronic facial nerve pain) or even arthritis in the neck can cause referred ear pain.
Recognizing the Symptoms Beyond the Ache
While pain is the most obvious sign, other symptoms can accompany it, offering clues to the underlying cause. Look out for:
- A feeling of fullness or pressure in the ear.
- Muffled hearing or temporary hearing loss.
- Discharge from the ear, which can be clear, yellow, green, or bloody.
- Fever, especially with infections.
- Ringing in the ears (tinnitus).
- Dizziness or problems with balance.
- In young children, irritability, trouble sleeping, and tugging at the ear are common signs.
When Should You See a Doctor?
Many cases of mild ear pain resolve on their own within a couple of days. However, you should seek medical attention if:
- The pain is severe or lasts longer than two to three days.
- You or your child has a high fever (over 102°F or 39°C).
- There is fluid, pus, or blood draining from the ear.
- You experience significant hearing loss, dizziness, or a severe headache.
- There’s swelling around the ear.
- For children under two, it’s always best to consult a doctor for ear pain.
In rare instances, persistent ear pain, especially when swallowing, could be a sign of a more serious condition like cancer, making a medical evaluation crucial.
Treatment Options for Ear Pain
The treatment for ear pain will depend on its underlying cause. Here are some common approaches:
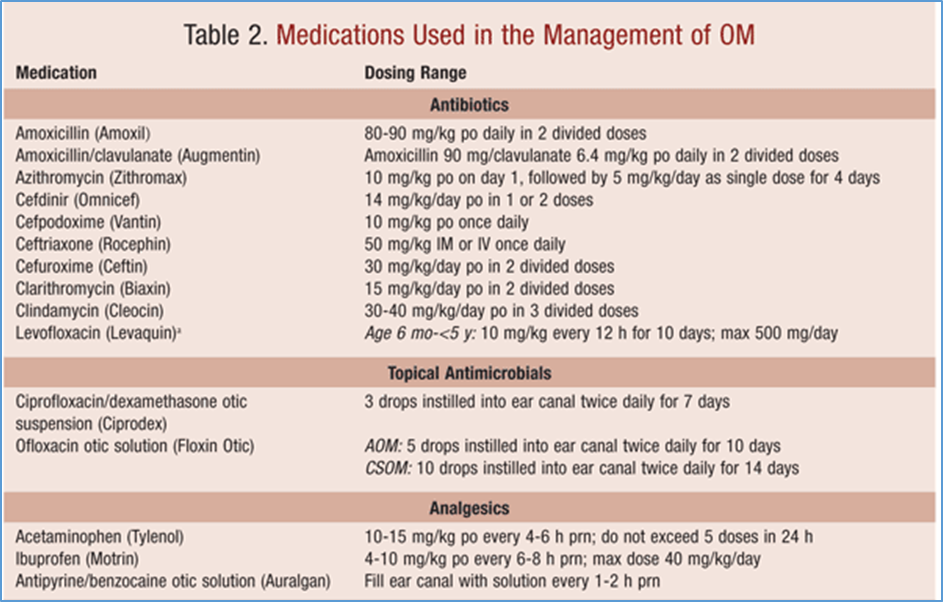
- Antibiotics for Infections
If an ear infection is diagnosed, antibiotics may be prescribed, particularly if it’s bacterial. Viral infections, however, do not require antibiotics and are usually managed with rest and hydration. - Pain Relievers
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate the pain associated with ear conditions. For children, ear drops formulated for pain relief may also be used, but always check with a pediatrician first. - Warm Compresses
Applying a warm compress to the affected ear can help soothe discomfort, especially for mild cases. It can also promote drainage if there’s any fluid buildup in the ear. - Ear Drops
For earwax buildup, over-the-counter ear drops can help soften the wax and make it easier to remove. Be sure to follow instructions carefully and avoid using these drops if you have a history of ear problems such as perforated eardrums. - Surgery
In rare cases, such as when fluid builds up behind the eardrum (in chronic otitis media), a doctor may recommend surgical intervention, such as the insertion of a small tube to help drain the fluid and prevent infection.
Preventing Future Ear Pain
While not all ear pain is preventable, these steps can reduce your risk:
- Keep Ears Dry: Use earplugs when swimming and dry your ears thoroughly after bathing to help prevent swimmer’s ear.
- Avoid Inserting Objects: Do not use cotton swabs or other objects to clean your ears, as this can push wax further in and potentially damage the eardrum.
- Manage Allergies and Colds: Treating cold and allergy symptoms can prevent the fluid buildup that often leads to middle ear infections.
- Stay Up-to-Date on Vaccinations: Childhood vaccinations can protect against some of the viruses and bacteria that cause ear infections.
- Clean Earbuds and Hearing Aids: Regularly clean any devices you place in your ears to prevent the introduction of bacteria.
In conclusion, while ear pain is a common ailment, understanding its potential causes is key to finding the right solution. For persistent or severe pain, a healthcare professional can provide an accurate diagnosis and a path to relief.
For more information, visit the American Academy of Otolaryngology.

