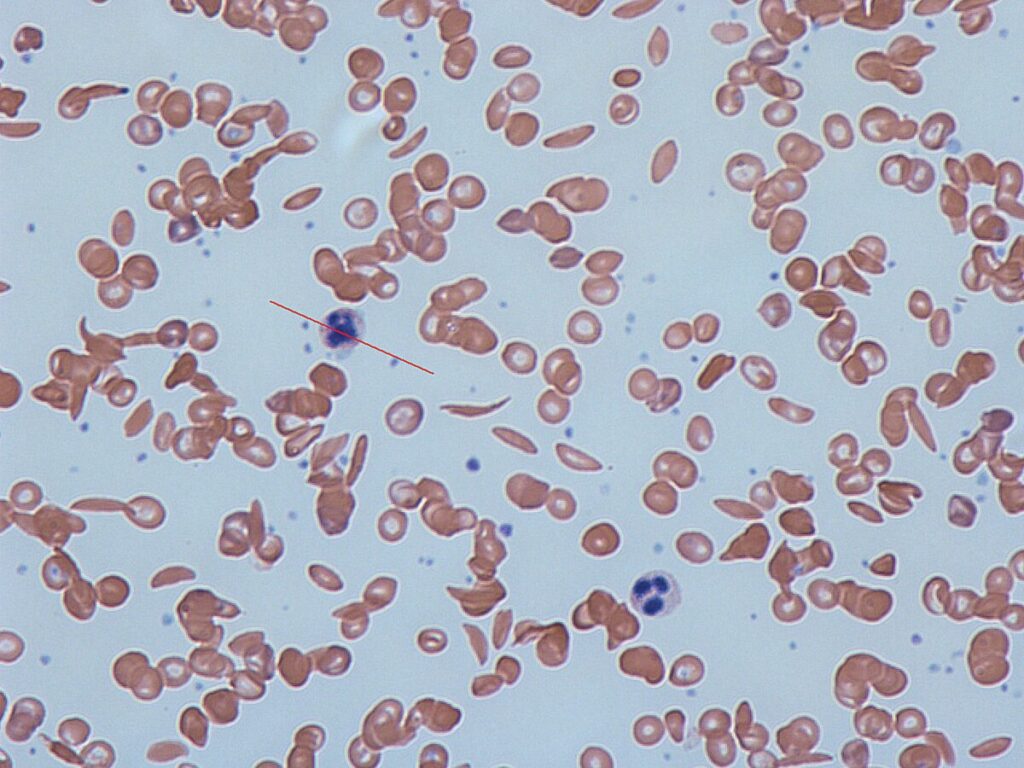
Sickle Cell Disease (SCD) is a genetic blood disorder that affects hemoglobin, the oxygen‑carrying protein in red blood cells. Due to a specific genetic mutation, these cells take on a crescent or sickle shape, making them less flexible and more prone to breaking. As a result, oxygen transport is reduced, and blood flow can be blocked.
According to the World Health Organization, millions of people worldwide live with SCD, with the highest prevalence in parts of Africa, India, and the Middle East. In some African regions, nearly half the population carries the sickle cell trait.
Causes of Sickle Cell Disease
SCD is inherited when a person receives the defective HBB gene from both parents. This genetic change replaces glutamic acid with valine in the beta‑globin chain of hemoglobin. Those with one copy of the gene are carriers and usually symptom‑free.
Symptoms of Sickle Cell Disease
Symptoms often begin in early childhood. Common signs include:
- Severe anemia and fatigue
- Pain crises (vaso‑occlusive crises)
- Swelling in hands and feet
- Frequent infections
- Delayed growth or puberty
- Vision problems
In addition, complications may occur. These include stroke, acute chest syndrome, organ damage, gallstones, and increased infection risk.
Complications:
•Due to blockage of splenic artery autosplenectomy occurs and spleen get destroyed which can increase risk of infections.
•Vaso-occlusive diseases like avascular necrosis of bone, acute chest syndrome, stroke, renal papillary necrosis(hematuria) etc.
•Can develop gall stones due to high unconjugated bilirubin
•Hepatic diseases, In >80% cases of SCD devlops hepatomegaly, hepatitis, intrahepatic cholestasis.
•Nephrotic syndrome
•Retinopathy
Diagnosis
- Early diagnosis improves outcomes. Tests include:
- Peripheral blood film to detect sickle‑shaped cells
- Hemoglobin electrophoresis (gold standard)
- Solubility test for screening
- Newborn screening, now mandatory in some Indian states
Treatment Options
Although there is no universal cure, treatment can greatly improve quality of life:
- Hydroxyurea to boost fetal hemoglobin (HbF)
- Voxelotor to improve oxygen binding
- Crizanlizumab to reduce blood cell clumping
- Folic acid for red cell production
- Pain relief using NSAIDs or opioids
- Blood transfusions for severe anemia
- Bone marrow transplant — a potential cure in eligible patients
- Gene therapy — under research but promising
Preventive care includes regular health check‑ups, CDC‑recommended vaccinations, and infection prevention measures.
Living with SCD
With proper care, people with SCD can live long, active lives. Supportive measures include:
- Balanced diet and hydration
- Regular exercise within safe limits
- Avoiding extreme temperatures and high altitudes
- Joining patient support groups for mental health
SCD in India
The disease is common in Madhya Pradesh, Maharashtra, Chhattisgarh, Odisha, Jharkhand, and Gujarat. In 2023, the Government of India launched the National Sickle Cell Elimination Mission to screen millions of people by 2047.
Conclusion
Sickle Cell Disease changes the shape of blood cells, but with awareness, early diagnosis, and consistent care, its impact can be reduced. By spreading knowledge and improving access to treatment, we can offer hope to millions living with this crescent‑shaped challenge.
Suggested External Links
(Place them naturally inside the article for credibility)

