
Hematuria is the medical term for the presence of red blood cells (RBCs) in the urine. It can appear in two forms:
- Gross hematuria – urine looks visibly red, pink, or tea-colored.
- Microscopic hematuria – blood is only detectable under a microscope, with more than 3 RBCs per high-power field (HPF).
A single test showing hematuria is not always serious. It can result from exercise, mild injury, menstruation, or allergies. However, persistent Blood in urine — such as more than 3 RBCs/HPF on three separate urinalyses, a single test with over 100 RBCs, or any gross hematuria — should be evaluated promptly, as it can indicate significant kidney or urinary tract disease.
Types of Hematuria
Blood in urine is classified based on when the blood appears during urination:
- Initial hematuria – Blood appears at the start of urination. Suggests a urethral source.
- Terminal hematuria – Blood appears at the end of urination. Suggests the bladder neck or prostatic urethra.
- Total hematuria – Blood is present throughout urination. Suggests a bladder, ureter, or kidney source.
Causes of Hematuria
Glomerular (Kidney Origin)
These conditions affect the kidney’s filtering units (glomeruli):
- Post-streptococcal glomerulonephritis
- IgA nephropathy
- Alport syndrome
- Lupus nephritis
- Vasculitis
Key Features:
Blood in urine with misshapen RBCs, RBC casts, and significant protein in urine (>500 mg/day) strongly points to glomerulonephritis. RBC casts form when red blood cells become trapped in protein molds inside the kidney’s tubules.
Non-Glomerular (Urological Origin)
These causes affect the urinary tract outside the kidney’s filtering system:
- Kidney or ureter stones
- Urinary tract infections (UTI), especially from Proteus or tuberculosis
- Bladder or kidney tumors
- Trauma
- Benign prostatic hyperplasia (BPH) in older men
- Acute cystitis or urethritis in women
- Strenuous exercise (transient hematuria)
- Anticoagulant medication overuse (e.g., warfarin)
Tip: Painless, visible hematuria in older adults — especially smokers — should be considered bladder cancer until proven otherwise.
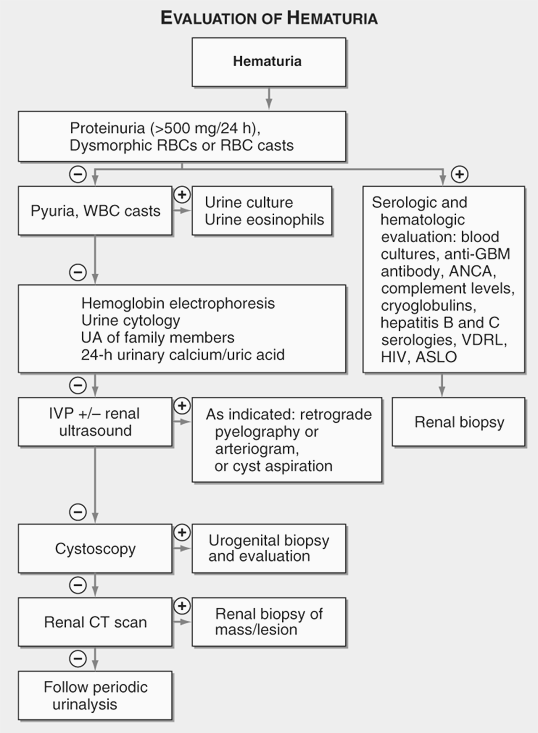
Diagnosis
A thorough evaluation is essential to find the cause:
- History & physical exam – Look for fever (infection), flank pain (stones), or risk factors like smoking (malignancy).
- Urine analysis – Check for RBCs, protein, and RBC casts.
- Urine culture – Detect infections.
- Ultrasound of kidneys, ureters, and bladder – Identify stones or masses.
- CT urography – Gold standard for assessing the upper urinary tract.
- Cystoscopy – Direct visualization of the bladder and urethra.
Clinical Pearls:
•In young adults, stones and UTI are common.
•In elderly, especially smokers, always rule out malignancy.
•Painless total Blood in urine = think bladder cancer until proven otherwise.
Management
Treatment depends on the underlying cause:
- Infections – Antibiotics after culture confirmation.
- Stones – Hydration, pain relief, and in some cases, surgical removal.
- Glomerular disease – Immunosuppressants or specific therapy.
- Tumors – Surgical or oncologic treatment.
- Medication-related bleeding – Adjust dosage or switch drugs.
Prevention and Follow-Up
- Stay hydrated to reduce stone risk.
- Avoid unnecessary use of blood-thinning medications.
- Treat UTIs promptly.
- Regular check-ups for people at higher risk (smokers, elderly).
Notice Title
Blood in urine is not a disease but a warning sign. While it may be harmless in some cases, it can also signal serious conditions like cancer or kidney disease. Prompt medical evaluation is the key to effective treatment and better outcomes.

