Understand the science behind chest pain, and when it could be a sign of something serious.
Overview: Why Chest Pain Deserves Attention:
Chest pain is a warning sign you should never ignore.
It’s one of the most common reasons people rush to the emergency room. Sometimes, it’s caused by something minor, like acid reflux or a pulled muscle. But in other cases, it could be your body’s cry for help.
Yes, chest pain can be deadly.
Heart attacks, pulmonary embolism, and even aortic dissection are some life-threatening conditions linked to chest pain. That’s why it’s crucial to know the difference between mild and serious causes.
Not all chest pain feels the same.
Some experience a sharp stabbing pain, while others feel pressure or tightness — like an elephant sitting on their chest. These differences can help doctors diagnose the real issue.
Your response time matters.
Quick action can mean the difference between recovery and a critical emergency. Understanding when to seek help is essential — especially if you’re at higher risk due to age, lifestyle, or medical history.
This guide will help you stay informed.
From causes and symptoms to treatments and home remedies, we’ll walk you through what chest pain means and when it’s time to call your doctor. Remember: Knowledge is power — but your doctor’s advice is essential..

❗ Disclaimer:
The information provided on Healnology is for educational purposes only and not a substitute for professional medical advice. Always consult your doctor before making health decisions or starting/stopping treatment.
❤️ Cardiac Causes of Chest Pain: Acute Coronary Syndrome (ACS):
One of the most critical concerns when evaluating chest pain is ruling out Acute Coronary Syndrome (ACS), which includes:
- Unstable angina
- ST-segment elevation myocardial infarction (STEMI)
- Non-ST segment elevation myocardial infarction (NSTEMI)
These conditions are linked to reduced blood flow to the heart, often due to a blocked artery.
Initial Assessment in the Emergency Department:
When a patient presents with chest pain, the following are the first steps in clinical evaluation:
1. Patient History
Doctors assess:
- Nature, duration, and radiation of the pain.
- Past medical history and risk factors like smoking, diabetes, or hypertension.
2. Physical Examination
- Blood pressure, heart sounds, respiratory exam.
- Look for signs of heart failure or shock.
3. Electrocardiogram (ECG)
- Detects ST-segment changes that may indicate myocardial infarction.
4. Cardiac Biomarkers (Troponin)
- Elevated troponin levels suggest heart muscle damage.
🧠 Decision Tools for Diagnosing Chest Pain:
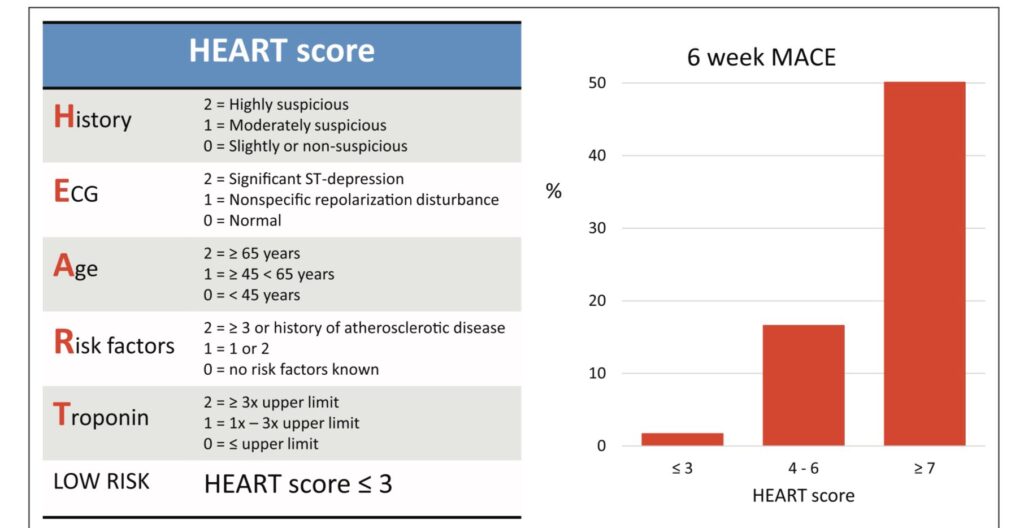
HEART Score
Used to evaluate the probability of ACS based on:
- History
- ECG
- Age
- Risk Factors
- Troponin levels
Score Interpretation:
- 0–3: Low risk
- ≥4: Not low risk
North American Chest Pain Rule
Patients are low-risk if they:
- Have no ischemic symptoms
- Normal ECG (According to the American Heart Association, early ECG can detect 50–70% of serious cardiac issues.)
- Age <50
- No history of coronary artery disease
- Normal troponin
These tools help doctors reduce unnecessary testing and hospital admissions.
Advanced Testing for Chest Pain
🧪 Stress Testing (TMT)
- Assesses heart function under stress.
- Useful in intermediate-risk cases.
- Can involve treadmill exercise or pharmacological stress agents.
🧲 CT Angiography
- Noninvasive method to detect coronary blockages.
- Helpful in low/intermediate-risk patients.
- Can also identify aortic dissection or pulmonary embolism.
🧲 Cardiac MRI (CMR)
- Offers detailed structural and tissue analysis.
- Effective in detecting recent infarcts or myocarditis.
- Best used in stable outpatient cases.
Outpatient Chest Pain: What You Need to Know
In outpatient settings:
- 20–40% of people report chest discomfort.
- Most are non-cardiac causes: reflux, muscle strain, anxiety.
- However, doctors should refer to the emergency department if ACS cannot be ruled out.
Critical Pathways in Hospitals
- Gastrointestinal: GERD, esophageal spasm, hiatal hernia
- Musculoskeletal: Costochondritis, rib fractures
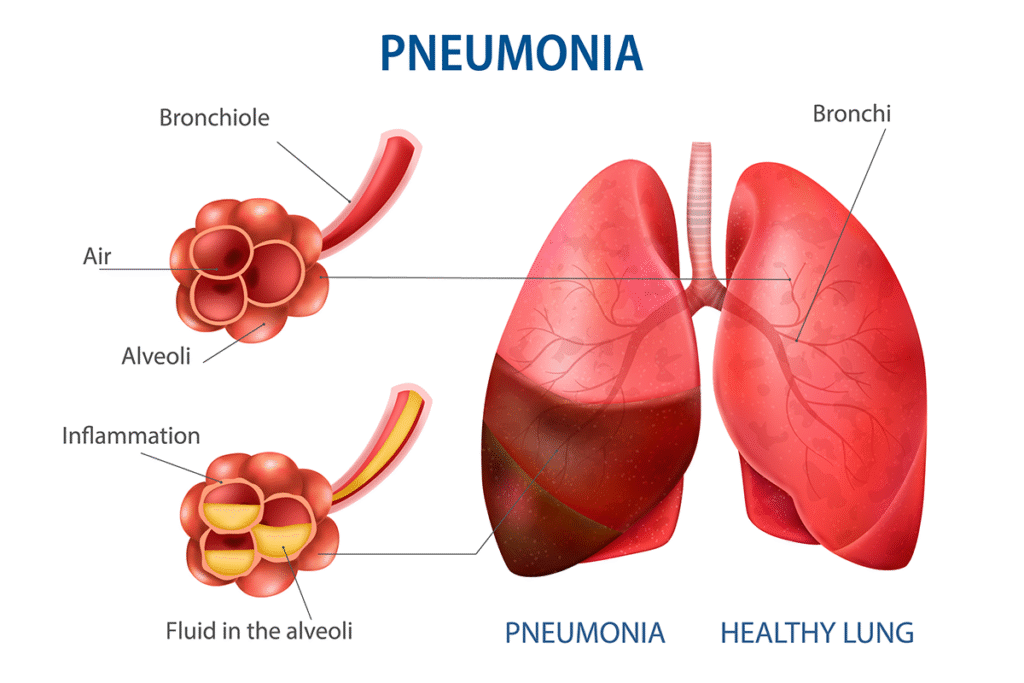
- Pulmonary: Pulmonary embolism, pneumothorax
- Psychological: Panic attacks, anxiety
When to Seek Immediate Medical Help
Call emergency services or go to the hospital immediately if you experience:
- Chest pain lasting more than 5 minutes
- Pain spreading to arm, jaw, or back
- Shortness of breath, dizziness, or sweating
- History of heart problems with new chest pain
Key Takeaways
Chest pain isn’t always a heart attack — but it should never be ignored.
Tools like the HEART Score and CT Angiography help identify risk.
Outpatient evaluation is safe for low-risk individuals, but emergency assessment is crucial when in doubt.
Timely diagnosis can save lives.
Conclusion
Chest pain should never be taken lightly. While not all chest pain is fatal, ignoring it can lead to severe outcomes. It’s vital to identify symptoms, know your risks, and consult a healthcare professional without delay. By staying informed and proactive, you can protect your heart and overall health.
Privacy Policy & Disclaimer:
Healnology’s content is for knowledge-sharing purposes only. We do not provide medical diagnosis or treatment advice.
Before acting on any health information:
- Talk to a qualified physician.
- Never delay or avoid treatment based on something you read here.
We do not collect any personal medical data unless explicitly submitted by the user.

Pingback: Pneumonia: Symptoms, Causes, Diagnosis & Treatment
Pingback: Dizziness and vertigo: Causes, Symptoms & When to Seek Help
Pingback: Headache Guide: Causes, Symptoms, Types & best Treatments
Pingback: Frequent Urination and Nocturia: Causes and Treatment
Pingback: AI Health Managers: The Future of Personalized Health