
Back pain isn’t just a symptom—it’s a modern epidemic. Whether you’re a student hunched over books, a desk-job warrior, or a fitness freak, back pain can strike anyone, anytime. But here’s the twist: you can manage—or even prevent—most back pain with the right knowledge.
Americans spend over $200 billion every year on chronic back pain.
Low back pain (LBP) ranks as the second most common reason for physician visits in the U.S.
Why Does Back Pain Happen?
The answer lies in your spine. This bony chain, which looks like a flexible caterpillar, protects nerves that carry pain signals throughout your body. When anything compresses these nerves, pain follows.
Nerve root injuries—like radiculopathy—often cause sharp pain in the neck, back, buttocks, or legs.
Common triggers for lower back issue include:
- Poor posture (that slouch is wrecking your spine)
- Muscle strain from sudden movements or overuse
- Herniated or degenerated discs
- Mental stress that tightens back muscles
- A sedentary lifestyle, lack of exercise, and obesity
- Bone disorders such as osteoarthritis, spondylolisthesis, ankylosing spondylitis
- Infections like spinal abscesses or vertebral osteomyelitis
- Conditions like osteoporosis or Paget’s disease that cause bone fractures
- Past injuries or spinal surgery
- Referred pain from abdominal or pelvic organs
Pain that starts in the spine can radiate to your buttocks or legs. Radicular pain, often sharp and shooting, travels along a nerve root from your lower back down to the leg.
Muscle spasms caused by spine disorders may also trigger dull, achy pain and an abnormal posture.
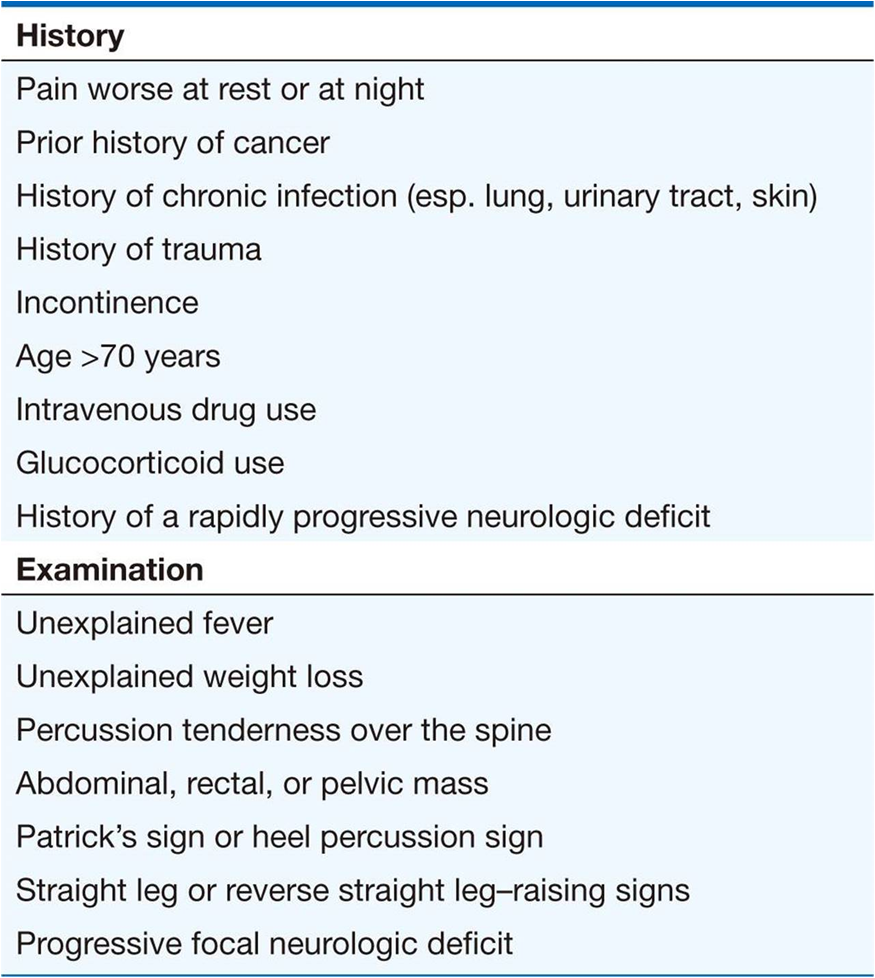
Red Flag Symptoms to Watch For
Seek immediate help if you notice:
- Pain radiating to your legs
- Numbness or tingling
- Difficulty walking or urinating
- Fever paired with lower back issue (possible infection)
•Yoga and core strengthening
Harvard research shows how yoga can relieve chronic this pain.
Medical Treatments for Back Pain
If pain doesn’t improve, seek expert care. Doctors often recommend:
- NSAIDs like acetaminophen or ibuprofen (don’t self-medicate!)
- Muscle relaxants like cyclobenzaprine (can cause drowsiness)
- Physiotherapy to improve strength and flexibility
- Epidural steroid injections for chronic or severe cases
- Short courses of oral steroids (like methylprednisolone) for disc-related nerve pain
- Surgery, but only for select conditions like herniated discs with nerve compression
- Opioids, only when strictly necessary
Understand the proper use and risks of NSAIDs from the FDA.
Did You Know?
Over 80% of adults will suffer from lower back issue at some point. But here’s the good news: most cases improve with simple lifestyle changes.
Final Words
Back pain may be common, but you don’t have to live with it. Care for your spine, and it will support you for a lifetime. If pain lingers or worsens, don’t wait—consult a doctor early. Timely care can prevent lasting damage.
WHO recommends regular physical activity for spine and overall health.
FAQ – Back Pain
Q1: Can stress cause back pain?
Yes, mental stress tightens muscles, especially in your neck and lower back.
Q2: Is back pain always due to spine issues?
Not always. Sometimes it’s referred from abdominal or pelvic organs.
Q3: When should I worry about back pain?
If you have numbness, fever, or difficulty walking—see a doctor right away.

