Discover the most common tick-borne diseases such as Lyme disease, Rocky Mountain spotted fever, and anaplasmosis. Learn symptoms, diagnostic methods, prevention strategies, and treatment options.
The Rising Threat of Tick-Borne Illnesses
Tick-borne diseases are a significant public health concern worldwide. Transmitted by the bite of infected ticks, these illnesses can lead to mild to severe systemic infections and, if untreated, may result in long-term complications or even death. With increasing tick populations due to climate change and human encroachment into wildlife habitats, understanding tick-borne infections is more important than ever.
What Are Tick-Borne Diseases?
Tick-borne diseases are infections caused by pathogens—bacteria, viruses, or protozoa—transmitted through the bite of infected ticks. While not all ticks carry disease, several species are vectors of multiple serious human pathogens.
Major disease-causing tick species include:
- Ixodes scapularis (Blacklegged/deer tick)
- Dermacentor variabilis (American dog tick)
- Amblyomma americanum (Lone star tick)
- Ixodes pacificus (Western blacklegged tick)
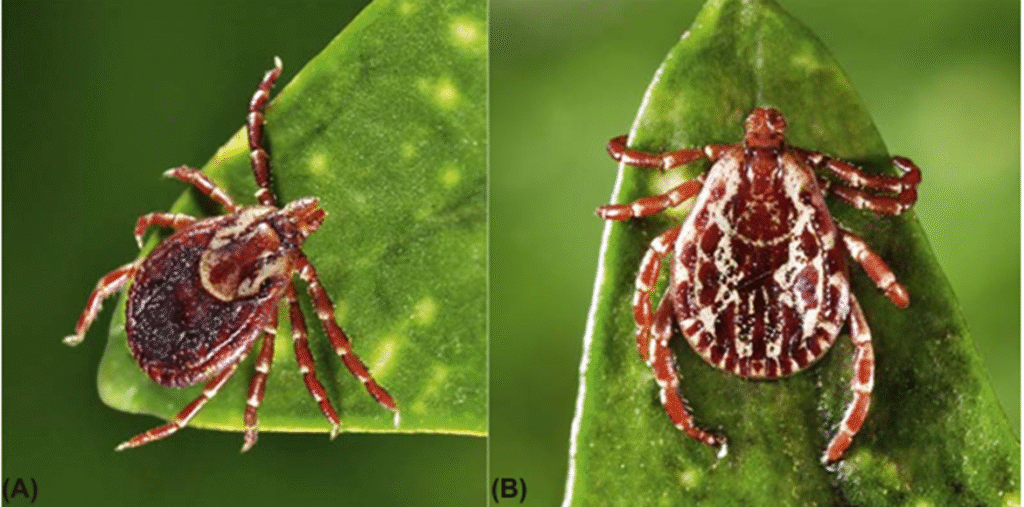
Dermacentor variabilis female & male
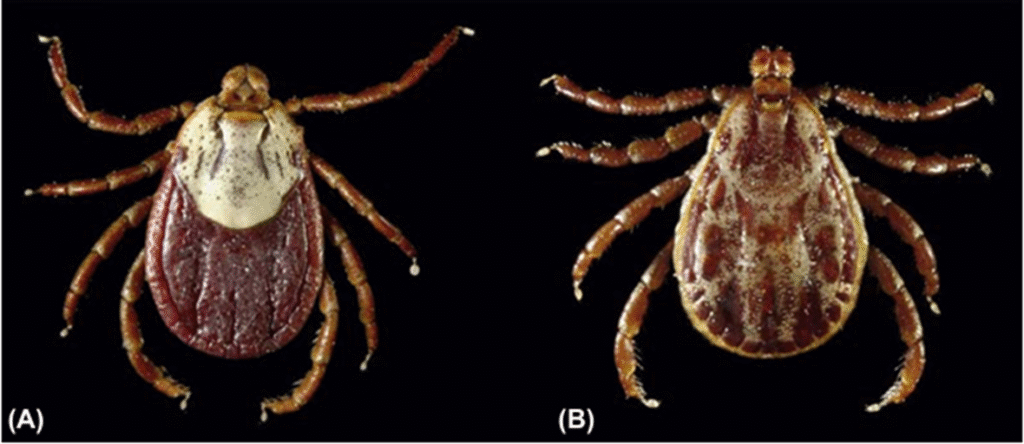
Rocky mountain wood tick D. andersoni

Ambyloma Americanum female & male
Common Tick-Borne Diseases
1. Lyme Disease
- Pathogen: Borrelia burgdorferi (occasionally Borrelia mayonii)
- Vector: Ixodes scapularis, Ixodes pacificus
- Geographic Distribution: Northeastern, north-central, and Pacific coastal U.S.
- Incubation Period: 3–30 days post-bite
- Clinical Presentation:
- Erythema migrans (bullseye rash)
- Fever, headache, myalgia, arthralgia
- Potential neurologic (facial palsy) and cardiac (AV block) involvement in later stages
- Diagnosis:
- Clinical presentation + serologic testing (ELISA followed by Western blot)
- Treatment:
- Early: Doxycycline (1st line), Amoxicillin or Cefuroxime (children/pregnant)
- Late: IV ceftriaxone for severe neuroborreliosis

Ixodes scapularis black legged female

Target rash Lyme disease
2. Rocky Mountain Spotted Fever (RMSF)
- Pathogen: Rickettsia rickettsia gram –ve coccobacili
- Vector: Dermacentor variabilis, D. andersoni
- Geographic Distribution: Southeastern and south-central U.S.
- Symptoms:
- High fever, severe headache, rash (typically starts on wrists/ankles)
- Nausea, vomiting, thrombocytopenia, hyponatremia
- Diagnosis:
- Clinical suspicion is critical (rash often absent in early disease)
- Serologic confirmation via indirect immunofluorescence assay (IFA)
- Treatment:
- Immediate doxycycline, regardless of patient age
- Delay in treatment increases mortality risk

Rocky mountain fever maculopapular rash
3. Anaplasmosis
- Pathogen: Anaplasma phagocytophilum
- Vector: Ixodes scapularis, I. pacificus
- Symptoms:
- Fever, malaise, leukopenia, thrombocytopenia, elevated liver enzymes
- Diagnosis:
- PCR of blood, peripheral smear (morulae in neutrophils), serology
- Treatment:
- Doxycycline (first-line therapy)

Western tick Ixodes pacificus
4. Ehrlichiosis
- Pathogens: Ehrlichia chaffeensis, E. ewingii
- Vector: Amblyomma americanum
- Symptoms:
- Fever, chills, malaise, leukopenia, thrombocytopenia, rash (more common in children)
- Diagnosis:
- PCR, serologic testing, blood smear
- Treatment:
- Doxycycline (prompt initiation is essential)
5. Babesiosis
- Pathogen: Babesia microti (protozoan)
- Vector: Ixodes scapularis
- Symptoms:
- Hemolytic anemia, fatigue, dark urine, hepatosplenomegaly
- Severe disease in asplenic, elderly, or immunocompromised patients
- Diagnosis:
- Peripheral blood smear (intraerythrocytic parasites), PCR, serology
- Treatment:
- Mild: Atovaquone + Azithromycin
- Severe: Clindamycin + Quinine
6. Powassan Virus Disease
- Pathogen: Powassan virus (Flavivirus)
- Vector: Ixodes scapularis
- Geographic Distribution: Northeastern U.S. and Great Lakes region
- Incubation: 1–4 weeks
- Symptoms:
- Fever, headache, vomiting, weakness
- Encephalitis, seizures, and long-term neurological deficits in severe cases
- Diagnosis:
- CSF analysis, PCR, IgM antibody testing via ELISA
- Treatment:
- No antiviral therapy available; supportive care in ICU settings
7. Kyasanur Forest Disease (KFD)
- Pathogen:
Caused by Kyasanur Forest Disease Virus (KFDV), a member of the Flavivirus family. - Vector:
Spread through the bite of infected ticks (Haemaphysalis spinigera). Monkeys act as amplifying hosts. - Geographic Distribution:
Endemic to South India, mainly Karnataka, with cases also reported in Kerala, Tamil Nadu, Goa, and Maharashtra. - Incubation Period:
3–8 days after a tick bite. - Symptoms:
Sudden fever, headache, muscle pain, vomiting, and sometimes bleeding. In some, a second phase occurs with neurological issues like tremors and confusion. - Diagnosis:
Confirmed through RT-PCR, ELISA, and other serological tests. - Treatment:
No specific antiviral; supportive care is essential. Hospitalization may be needed in severe cases. - Prevention:
Vaccination in endemic areas, tick bite prevention, and public awareness during outbreaks.
8. Tularemia
- Pathogen:
Caused by the bacterium Francisella tularensis – a highly infectious, gram-negative bacterium. - Vector & Transmission:
Spread by:- Ticks, deer flies
- Direct contact with infected animals (especially rabbits, rodents)
- Inhalation of contaminated dust
- Ingestion of contaminated water or food
- Geographic Distribution:
Found in North America, parts of Europe, and Asia. Rare but potentially severe. - Incubation Period:
3–5 days (can range from 1–14 days). - Symptoms:
Varies by form; common types include:- Ulceroglandular: Skin ulcer at infection site + swollen lymph nodes
- Glandular: Swollen lymph nodes without ulcer
- Oculoglandular: Eye irritation and swelling
- Pneumonic: Cough, chest pain, and difficulty breathing (inhalation form)
- Typhoidal: General illness with high fever and sepsis-like symptoms
- Diagnosis:
Confirmed by serological tests, PCR, or culture (handled in specialized labs due to high infectivity). - Treatment:
Treated effectively with antibiotics like streptomycin, gentamicin, doxycycline, or ciprofloxacin. - Prevention:
- Avoid contact with wild animals
- Use insect repellents and protective clothing
- Cook meat thoroughly
- No widely available vaccine yet
9. Tick-Borne Encephalitis (TBE)
- Pathogen:
Caused by the Tick-Borne Encephalitis Virus (TBEV)
Belongs to the Flavivirus family (same as dengue and Zika viruses). - Vector:
Transmitted by infected ticks, mainly:- Ixodes ricinus (Europe)
- Ixodes persulcatus (Asia)
- Geographic Distribution:
Common in parts of Europe, Russia, and Asia, especially forested areas during spring to early autumn. - Incubation Period:
Usually 7–14 days after a tick bite. - Symptoms:
Biphasic illness (two phases):- First phase: Flu-like symptoms – fever, fatigue, headache, muscle pain.
- Second phase: In some cases – neurological symptoms such as:
- Meningitis (headache, stiff neck)
- Encephalitis (confusion, seizures)
- Paralysis (rare but severe)
- Diagnosis:
Confirmed by IgM/IgG ELISA, PCR, or CSF analysis (in neurological cases). - Treatment:
- No specific antiviral
- Supportive care (fluids, pain relief, hospitalization if severe)
- Prevention:
- TBE vaccine available in endemic countries (especially Europe)
- Avoid tick bites: wear long clothing, use repellents, check for ticks after forest visits
- No raw milk from goats or sheep (can transmit virus)
10. Tick Typhus
- Pathogen:
Caused by Rickettsia bacteria (mainly Rickettsia conorii in India, R. rickettsii in the Americas). - Vector:
Transmitted by tick bites, especially from:- Rhipicephalus sanguineus (brown dog tick)
- Dermacentor or Amblyomma species (varies by region)
- Geographic Distribution:
Found worldwide; common in:- India (known as Indian Tick Typhus)
- Africa (Mediterranean spotted fever)
- USA (Rocky Mountain Spotted Fever)
- Australia (Queensland Tick Typhus)
- Incubation Period:
5–7 days after tick bite - Symptoms:
- High fever
- Severe headache
- Muscle pain
- Rash (spotted, often starts on limbs and spreads)
- Eschar (black scab at tick bite site in some cases)
- Lymphadenopathy
- If untreated, may lead to serious complications (organ failure, encephalitis)
- Diagnosis:
- Clinical suspicion based on fever + rash + tick exposure
- Confirmed by serology (Weil-Felix test), ELISA, or PCR
- Treatment:
- Doxycycline is the drug of choice (even for children)
- Early treatment significantly reduces risk of complications
- Prevention:
- Avoid tick exposure: protective clothing, repellents
- Tick checks after outdoor activity
- Control of dogs and rodents that host ticks
Clinical Symptoms of Tick-Borne Illnesses
While symptoms vary by disease, common early manifestations include:
- Fever and chills
- Headache and fatigue
- Myalgia (muscle aches) and arthralgia (joint pain)
- Rash (disease-specific)
- Neurological signs: confusion, ataxia, cranial nerve palsy (in late stages)
Note: Co-infection with multiple tick-borne pathogens is possible (e.g., Lyme + Babesiosis).
Diagnostic Approach
1. History and Exposure Assessment
- Recent outdoor activity in endemic areas
- Time spent in wooded, grassy, or brushy environments
2. Laboratory Investigations
- Complete blood count (CBC): May show leukopenia, thrombocytopenia
- Liver function tests (LFTs): May reveal elevated transaminases
- Serology and PCR: Specific to pathogen suspected
- Peripheral smear: Useful for Babesiosis and Ehrlichiosis
Tick-Bite Prevention Strategies
Personal Protective Measures
- Wear long-sleeved clothing and tuck pants into socks
- Apply EPA-registered tick repellents (e.g., DEET, picaridin)
- Treat clothing and gear with permethrin
- Shower within two hours of outdoor activity
- Conduct full-body tick checks daily (especially underarms, groin, scalp)
Tick Removal Protocol
- Use fine-tipped tweezers to grasp tick close to skin
- Pull upward with steady pressure (do not twist)
- Disinfect area with alcohol or iodine
- Do not use petroleum jelly, matches, or nail polish
When to Seek Medical Attention
Consult a healthcare provider immediately if:
- A tick bite is followed by fever, rash, or joint pain
- Neurologic symptoms (e.g., confusion, facial paralysis) appear
- You live in or recently traveled to a tick-endemic area
- A partially removed tick was embedded for an extended period
Conclusion: Medical Vigilance Is Key
Tick-borne diseases can be severe but are largely preventable and treatable with early diagnosis and proper intervention. Clinicians and the public should maintain high awareness, especially during peak tick activity months (spring through fall). Preventive measures, prompt removal of ticks, and timely medical care are crucial in mitigating risks.

